solarchat.org – Modern healthcare increasingly depends on evidence, and research physiotherapy now sits at the center of this shift. Instead of relying only on tradition or habit, clinicians are turning to data, trials, and rigorous analysis to guide every decision. Patients benefit from safer care, clearer goals, and treatment that adapts as new findings emerge.
In this evolving landscape, research physiotherapy helps bridge the gap between theory and real-life clinical practice. Therapists can examine which exercises, manual techniques, and technologies deliver meaningful results. This approach offers a reliable pathway for both faster recovery and better long-term function.
As more clinics adopt evidence-focused methods, the profession becomes more accountable and transparent. Research physiotherapy is no longer a specialized niche but a driving force behind innovation. Understanding how it works can help patients, students, and clinicians make decisions that genuinely improve outcomes.
How Research Physiotherapy Shapes Clinical Assessment
Accurate assessment is the foundation of any successful rehabilitation program, and research physiotherapy refines this crucial step. Well-designed studies compare different tests, screening tools, and measurement techniques to determine which are most reliable. As a result, clinicians are less likely to miss key impairments or misinterpret symptoms.
Validated outcome measures now guide how therapists track progress and adjust plans. Instead of vague impressions, research physiotherapy supports structured questioning, standardized tests, and clear baselines. This makes it easier to spot meaningful change and to communicate results with patients and other professionals.
Assessment methods informed by research also help identify red flags that require urgent medical review. For example, certain neurological signs or unexplained pain patterns may signal serious conditions. By following evidence-backed protocols, physiotherapists improve safety and ensure timely referrals when needed.
Key Principles Behind Research Physiotherapy Assessment
Several core ideas shape assessment strategies emerging from research physiotherapy. Reliability, which describes how consistent a test is over time or between clinicians, is carefully evaluated. Validity, the extent to which a test measures what it claims to measure, is equally crucial.
Researchers also examine responsiveness, or how well a test detects meaningful clinical change. When clinicians choose tools with strong evidence in these areas, they gain more confidence in the results. This precision supports smarter treatment planning and more accurate prognoses.
Another important concept is feasibility, meaning whether a test is practical in real-world settings. Research physiotherapy recognizes that complex tools are useless if they take too long or demand expensive equipment. Studies therefore balance scientific rigor with day-to-day clinical realities.
Using Technology in Evidence-Based Assessment
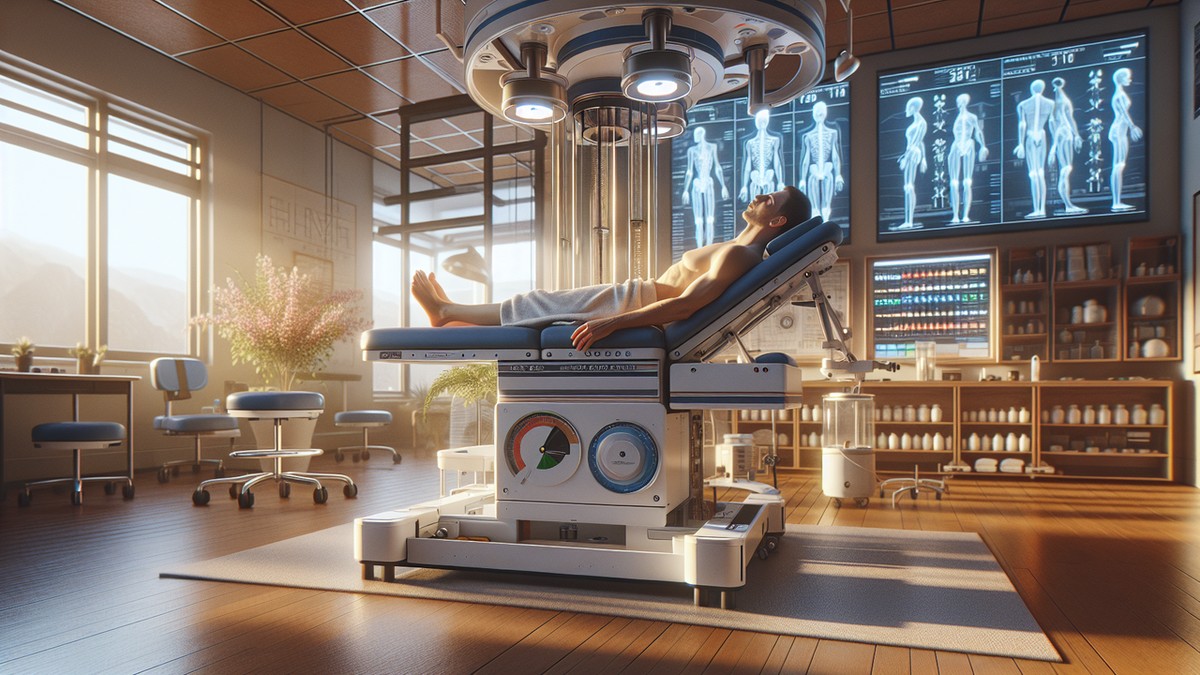
Advances in digital technology are reshaping the role of assessment in research physiotherapy. Motion analysis systems, wearable sensors, and smartphone applications now collect data that once required laboratory settings. These tools provide real-time insight into gait, posture, and muscle activation.
Collected data can then be compared across large patient groups, revealing patterns not visible to the naked eye. Research physiotherapy uses this information to refine diagnostic categories and understand subtle biomechanical differences. Over time, this can lead to highly individualized treatment plans.
Telehealth platforms also contribute to better assessment, especially in remote regions. Clinicians can observe movement via video and use validated questionnaires delivered online. While not a full replacement for in-person visits, these tools expand access to evidence-informed care.
From Assessment to Measurable Goals
Evidence-based assessment naturally flows into structured goal setting, another focus of research physiotherapy. Studies highlight the benefit of goals that are specific, measurable, and time-bound. Patients who understand these targets tend to stay more engaged and motivated.
Clinicians can translate test findings into functional aims, such as walking a set distance or returning to a sport. Research physiotherapy emphasizes linking goals to meaningful daily activities rather than only clinical numbers. This function-first mindset leads to more relevant rehabilitation strategies.
By revisiting the same validated measures over time, therapists can show objective progress toward each goal. If improvement stalls, evidence-based guidelines suggest alternative strategies or further investigation. This feedback loop anchors rehabilitation in data while still respecting individual differences.
Research Physiotherapy and Evidence-Based Treatment Planning
Beyond assessment, research physiotherapy strongly influences how treatment plans are built and refined. Randomized trials, systematic reviews, and clinical guidelines reveal which interventions work best for specific conditions. This evidence helps clinicians avoid outdated methods that consume time without clear benefit.
For musculoskeletal problems, for example, exercise therapy often has strong support. Research physiotherapy helps define optimal dosage, intensity, and progression stages. Patients gain a structured program rather than a random collection of exercises.
In neurological rehabilitation, studies may highlight the value of task-specific training or constraint-based approaches. Research physiotherapy ensures that these strategies are used appropriately and combined with other relevant methods. The result is a plan grounded in both science and clinical experience.
Choosing the Right Interventions Through Research Physiotherapy
A common challenge in practice is deciding which technique to prioritize when time is limited. Research physiotherapy addresses this by ranking interventions according to strength of evidence. High-quality trials and meta-analyses carry more weight than small or poorly controlled studies.
Clinicians can consult clinical practice guidelines that compile these findings into practical recommendations. While not rigid rules, these guidelines help therapists select approaches with the best support. This reduces guesswork and makes treatment more predictable.
Importantly, research physiotherapy never removes the need for individual judgment. Therapists still adapt protocols to each person’s age, comorbidities, and preferences. Evidence provides a strong starting point, but clinical reasoning ensures appropriate application.
Monitoring Outcomes and Adjusting Treatment
Ongoing outcome monitoring is central to research physiotherapy and vital for successful recovery. By repeating key measures at regular intervals, clinicians can see whether a treatment is working. If results are below expectations, they can revise the plan early rather than waiting.
This adaptive approach aligns with modern ideas of precision rehabilitation. Instead of rigidly following a preset protocol, therapists change intensity, frequency, or technique according to progress. Research physiotherapy supports these decisions by highlighting which modifications are likely to help.
Patients benefit from transparent discussions about their results, which can improve adherence. When individuals see measurable gains, they often commit more fully to home exercise. Conversely, limited progress may prompt constructive conversations about barriers and new strategies.
Integrating Patient Values into Evidence-Based Care
High-quality care demands more than strong research alone; it must also align with patient values. Modern research physiotherapy places shared decision-making at the heart of treatment planning. Clinicians present evidence, explain options, and then consider what matters most to each person.
For example, one patient might prioritize returning to competitive sport quickly, while another values pain relief for daily work. Research physiotherapy ensures that both scenarios can be guided by data-driven techniques. However, the chosen route will differ to match personal preferences.
When people feel heard and involved, adherence improves and satisfaction rises. Studies consistently link collaborative planning with better outcomes. Evidence, professional judgment, and patient goals together form a powerful, balanced approach.
The Future of Research Physiotherapy in Everyday Practice
The influence of research physiotherapy will likely increase as healthcare continues to value measurable outcomes. New technologies, larger data sets, and international collaborations are accelerating discovery. These changes offer opportunities for more precise and personalized rehabilitation programs.
Digital record systems now allow clinics to contribute anonymized data to large registries. Research physiotherapy can then analyze real-world results, complementing controlled clinical trials. This blended evidence base reflects both ideal conditions and everyday complexity.
As findings accumulate, continuous professional development becomes essential. Clinicians who engage with current research are better equipped to refine their methods. Ongoing learning ensures that practice remains current rather than drifting into outdated habits.
Education and Training in Research Physiotherapy
Physiotherapy education increasingly emphasizes research literacy, preparing new graduates to interpret scientific work. Students learn how to read studies, judge quality, and apply findings thoughtfully. This foundation allows them to join the broader research physiotherapy community as informed practitioners.
Postgraduate courses and specialist programs continue this development. Clinicians can focus on areas such as sports, neurology, or cardiorespiratory care, guided by current evidence. Regular exposure to new findings keeps their skills evolving.
Mentorship and journal clubs inside clinics further embed an evidence-focused culture. By discussing studies together, teams learn to critique methods and share practical insights. This cooperation turns research physiotherapy from an abstract concept into daily routine.
Collaborative Research Between Clinics and Universities
Stronger partnerships between healthcare settings and academic institutions are reshaping research physiotherapy. Clinicians bring real-world questions, while researchers offer methodological expertise. Together, they design projects that directly address everyday challenges.
Such collaborations might test new exercise programs, investigate novel technologies, or refine assessment tools. Research physiotherapy benefits when these studies use realistic patient populations and clinical constraints. The findings, in turn, inform local practice and contribute to international knowledge.
Patients often welcome the chance to participate, knowing their input may help others in future. Ethical oversight and informed consent ensure safety and transparency. These projects strengthen trust in both the profession and the scientific process.
Empowering Patients Through Accessible Evidence
As information becomes easier to access, patients increasingly ask for clear, research-based explanations. Research physiotherapy responds by translating complex findings into understandable language. Educational materials, workshops, and digital resources all play a role.
Well-informed patients can better judge treatment claims and avoid unsupported trends. When they understand why certain exercises or techniques are chosen, motivation to follow through often improves. Transparency around evidence also reduces confusion when recommendations change over time.
By combining trustworthy information with compassionate guidance, clinicians help people take an active role in recovery. This partnership reflects the true spirit of research physiotherapy: science in service of meaningful, individual change.